
As of 2015, 3.4 million Americans carried a diagnosis of epilepsy with 150,000 new diagnoses annually. Nearly a third of those will have intractable epilepsy, which means seizures continue despite medication treatment.
Ketogenic Metabolic Therapy (KMT), a high fat, low carbohydrate diet, provides a new option and new hope for those with intractable epilepsy. About half of patients who participate in #Ketogenic Metabolic Therapy clinical trials experience at least a 50% reduction in seizures and about 1 in 7 become seizure-free. Additionally, many patients report improved alertness, cognition, and interaction.
How KMT works is not entirely known, but we do know that the process of burning fat (ketosis) instead of carbohydrates for energy reduces inflammation, increases antioxidant production, boosts efficiency in energy production and increases production of a brain chemical called GABA. The end result for patients is a decrease in seizures.
Keto may be the latest weight loss trend, but KMT is not your Pinterest Keto. For people with intractable epilepsy, KMT is calculated to meet individual nutrition needs and is closely monitored by an epileptologist and dietitian for safe and effective management. Without appropriate monitoring, there is increased risk for side effects such as poor growth, electrolyte abnormalities, nutrient deficiencies, kidney stones and decreased bone density. Rare, but more serious, side effects include heart arrhythmias, liver dysfunction or pancreatitis.
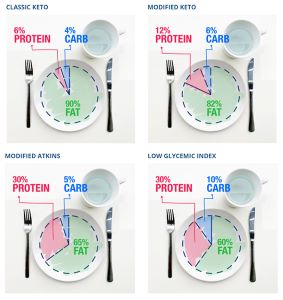
KMT can be modified for different ages and nutritional needs. There are options available for tube feeds as well as oral diets. The graphic below shows some of the variations offered at Phoenix Children’s Hospital.
While the keto-hype has led to a variety of ready-to-eat low-carb foods, many of these options still fall outside of the carbohydrate allotment for KMT. However, our dietitians have more than 20 years of combined experience managing patients on KMT. We can modify favorite foods and recipes to meet individualized KMT nutrition goals and manage seizures.
While dietary changes can be difficult, one grateful family said, “The keto way is better than the seizure way.”
At Phoenix Children’s Hospital, our Ketogenic Program is made up of a multi-disciplinary team trained in KMT from specialty areas including Neurology, Nutrition, Pharmacy and Psychology. We understand the unique challenges that dietary therapies pose to the family unit. To provide the best possible support to families, we have developed and provide resources needed for successful implementation and management of KMT.
KMT may not be safe to use with certain conditions or medications. If you think that KMT may be a treatment option for you or your child, contact your neurologist for a referral.
For additional resources on KMT, visit:
