When baby Jacquie was born, her parents were advised to take their daughter to the pediatrician: Her newborn screening results had revealed she likely had Sickle Cell Anemia, a genetic blood disorder. At nine months old, Jacquie was hospitalized with a high fever and her first pain crisis – but that hasn’t slowed her down.
Despite a rough start in life, Jacquie is like other toddlers: She loves dance parties in her living room, splashing in the pool, acting like a goofball and bringing laughter to her loved ones.




During Sickle Cell Awareness Month in September, Phoenix Children’s is celebrating patients like Jacquie and generating awareness of the condition.
What is Sickle Cell Disease?
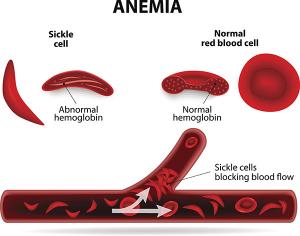
In sickle cell disease, hemoglobin (which carries oxygen to the tissues) is abnormal. As a result, the red blood cells that hemoglobin inhabits are shaped like a sickle rather than a disc. The sickle cells will “get stuck” and block the flow of blood and oxygen to vital organs and extremities. This lack of blood flow causes pain crises and makes it harder to filter out viruses and bacteria. In addition, sickle cell can lead to a number of problems like anemia, chronic pain, fatigue and stroke.
Today, most children are screened for sickle cell during regular newborn screenings, but they might not show symptoms of the disease for up to a year. When they do come, symptoms may include jaundice (skin yellowing), anemia and sudden pain—especially in the chest, arms and legs.
Every year, 24,000 babies are born with sickle cell in the U.S. The condition isn’t contagious, though it is hereditary and most prevalent in Black and Latinx communities. In fact, it’s estimated that in the U.S., 8% of people of African descent, which includes Black Americans, carry the sickle cell trait.
How do you treat children with sickle cell?
Because patients with sickle cell face a wide range of potential complications, the Sickle Cell Program at Phoenix Children's Hospital provides comprehensive care all under one roof. Our team of physicians, nurse practitioners, nurse coordinators, social workers, medical assistants and administrative assistants create individualized care plans for each patient to help manage symptoms and avoid long-term complications.
In partnership with Phoenix Children’s award-winning IT department, the Sickle Cell team created and utilizes a Sickle Cell dashboard that builds in best practices and provides clinician prompts based on each patient’s unique symptoms and prognosis. The care team utilizes data to inform state-of-the-art sickle cell care, which may include immunizations, preventive scans, and therapies such as Hydroxyurea, L-glutamine, Voxelotor and Crizanlizumab.
And, because many sickle cell patients struggle with pain, we work with the Phoenix Children’s Pain Medicine team to take advantage of the most recent American Society of Hematology guidance for pain management in sickle cell and improve comfort and care for hospitalized patients who experience pain episodes.
What’s the prognosis for kids with the disease?
There are four types of sickle cell. The type of sickle cell, along with child’s age, other health conditions and tolerance for therapies influence the severity of side effects. Medical breakthroughs have improved the course of care for children and reduced the chances for serious complications from the disease. Still, it remains a chronic and potentially life-threatening condition that requires close monitoring.
While there is no universal cure for sickle cell disease, our cell therapy team has successfully cured the condition through stem cell transplants. The team is also capable of providing haplo-identical stem cell transplant, which will expand access to this curative therapy to many more sickle cell patients.
As part of the Phoenix Children’s Center for Cancer and Blood Disorders’ commitment to leading advancements in sickle cell research, our team is part of the Pacific Regional Sickle Cell Consortium and the American Society of Hematology Clinical Trials Network.
