How prenatal diagnosis of clubfoot makes a difference for a lifetime

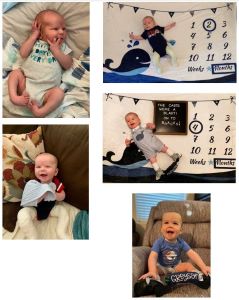
When parents first meet orthopedic surgeon and clubfoot specialist, Jessica Burns, MD, they immediately take note of her soothing voice and calming manner, said Kaitlyn, the mother of Greyson, now 18 months old, who was born with severe bilateral clubfoot (meaning both feet were involved). As Dr. Burns explained the detailed treatment process to them, they also quickly noted her deep expertise.
“We learned Greyson’s diagnosis early – during an ultrasound at 20 weeks – and we were very scared,” Kaitlyn said. “We didn’t know anything about clubfoot. When we were ultimately assigned to Dr. Burns for care, she took a great deal of time to explain everything, reassured us that effective treatment is available and gave us a detailed timeline. There is something about her calm, thorough manner that helped relieve my stress, and I am very grateful for her support – every step of the way.”
What is clubfoot?
About one in 1,000 babies in the U.S. is born with clubfoot, a birth defect that turns one or both feet inward, affecting the bones, muscles, tendons and blood vessels. Without treatment, children will likely learn to stand and walk, but they will ultimately experience considerable functional disability and pain as they grow older. With treatment, however – particularly with early intervention – children can live active lives, participate in typical childhood activities and even play sports.
The most common type of clubfoot is “isolated,” meaning the child has no other medical conditions. “Non-isolated” clubfoot is associated with other issues such as spina bifida. Greyson’s clubfoot was isolated.
Why is prenatal diagnosis so important?
What excites Dr. Burns today is that radiologists who perform prenatal ultrasounds can now identify clubfoot very early, and with further testing, doctors can also determine its specific type.
“Traditionally, clubfoot was diagnosed at birth or even later in infancy, and parents were referred to a pediatric orthopedist for their child’s care,” she explained. “This caused tremendous stress and worry. Parents were excited to be welcoming their new baby into the world, but they were also suddenly facing fear and confusion about the diagnosis with no preparation.
“Now, as ultrasound technology has advanced and images have become clearer, radiologists can identify clubfoot prenatally with greater accuracy,” she continued. “This means we can shift from a potential diagnosis to very early education of parents ahead of birth. It’s a beautiful progression; we can prepare parents about what to expect, establish trusted relationships and move right into treatment after birth, which is the most effective approach.”
Treatment as sculpting: the “Ponseti Method”
“There are some common misperceptions about clubfoot and its treatment,” explained Dr. Burns. “Many people think that children have to undergo multiple surgeries and will have life-long physical limitations. That’s definitely not true.”
At Phoenix Children’s and other centers worldwide, specialists now use the Ponseti method, named after Ignacio Ponseti, MD, of the University of Iowa. He developed the massage-stretch-cast approach, followed by long-term bracing, which has become the standard of care. While this method can take up to five years, most children with clubfoot avoid major surgery and have excellent long-term results.
At every stage, the team of experts at Phoenix Children’s works closely with patients and families, providing care, education, specialized technology and support. This team includes orthopedic surgeons like Dr. Burns; orthopedic technicians who participate in the casting phase; specially trained clinical nurses; and orthotists who specialize in creating the shoes and braces for the final phase of care.
Stage one, massage-stretch-cast, began for Greyson at two weeks of age.
“The foot is almost completely made of cartilage, so at this very early stage of treatment, we have an amazing opportunity to mold babies’ tiny little feet into a different shape and to move them into the right position,” said Dr. Burns. “We massage and stretch very gently, one step at a time. It’s not painful, but it’s important for babies to be as relaxed as possible during treatment. Parents often feed their children as I do this massaging and stretching to help keep them calm.”
After each session, toe-to-thigh casts are placed on the foot (or both feet in Greyson’s case) to hold the new position.
“Early on, this stage was a little easier than we expected because Dr. Burns was so good at preparing us and putting all of us at ease,” said Kaitlyn. “My husband, Zach, fed Greyson during casting, and it went pretty smoothly. Unfortunately, it got a little harder as Greyson got older. He developed some red marks from the casts, and his feet regressed a bit, so it took 10 casts over a full three months, rather than the usual four to six casts. But we made it to the next stage.”
Just before the final casting, Dr. Burns performed an outpatient surgical procedure called a tenotomy on both of Greyson’s heels. During the procedure, a small cut was made in each Achilles tendons to allow them to grow to their normal length by the time the last casts were removed.
The next stage – referred to as “B and B” for braces and bars – is the longest. Greyson was fitted with special shoes attached to a metal bar that kept his feet the proper distance apart and at the correct angle. He wore the braces 24 hours a day for 3 months, then 16 hours per day, and he is now wearing them between 12 and 14 hours per day.
“Bracing is critical,” said Dr. Burns. “Clubfoot can recur in 80 to 90 percent of children if they don’t wear their braces. Kaitlyn and Zach were excellent with compliance, and I know this is not an easy phase for patients or parents. But it has made a world of difference for Greyson. He is doing extremely well.”

“Greyson is so resilient,” said Kaitlyn. “I probably kept the braces and bars on longer than I was even supposed to because I was so terrified of regression. But Greyson learned to crawl and stand, and now he’s walking by holding on to things. His gross motor skills are only mildly delayed. And he’s a happy child. He loves to talk and laugh. He really makes us smile!”
Dr. Burns shared that early diagnosis of clubfoot has significantly improved the experience for parents and the outcomes for children.
“I love knowing that there is something we can do for a child with clubfoot,” she said with a huge smile. “We have a way to correct it. We have a treatment process that truly makes a difference for a lifetime. There is nothing more rewarding than seeing a child be able to get around and interact with their environment in a positive way. My patients are my inspiration.”
