Most people don’t realize that children and young adults can get skin cancer too. May is Skin Cancer Awareness/Melanoma Awareness Month, and we don’t want to leave our younger patients out of the melanoma ‘convo.’ Although not as common as in adults, melanoma is the second most common cancer in ages 15-29 years old! Yes, you read correctly—teenagers and young adults are at highest risk of those in the pediatric population.
Know the facts:
- Melanoma in children accounts for 1-4% of melanomas overall and 4% of all cancer diagnosed in older children. More than 400 cases of melanoma are diagnosed each year in the US in patients younger than 20 years of age.
- Even one blistering sunburn in childhood or adolescence more than doubles your chance of getting melanoma later in life; and the risk of melanoma more than doubles with more than 5 sunburns.
Risk factors for your child to develop melanoma
Although it isn’t always clear why some cases of pediatric melanoma occur, we know that a family history of melanoma and atypical appearing moles, significant sun exposure (UV radiation), tanning bed use, having a large number of moles or large/giant moles (also called nevi), having fair skin (blonde/red hair and blue eyes), a tendency to sunburn, a previous history of immunosuppression or low immune system conditions, and certain inherited conditions like xeroderma pigmentosum, that increase the risk of early onset cancers, can make it more likely your child will develop a melanoma. If your child has any of these risk factors, we recommend you make an appointment with a board-certified pediatric dermatologist.
There are several types of melanoma that can occur in children and young adults—conventional ‘adult type melanoma’, melanoma arising in a large/giant nevus, and Spitz/spitzoid melanoma, are some of them. It is important for parents and caregivers to note that pediatric melanomas are often underdiagnosed or misdiagnosed (up to 40% of the time) and this causes a delay in getting diagnosed and treated.
How to not miss it:
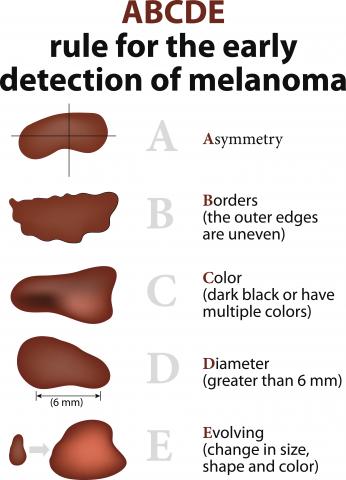
- Know the typical “ABCDEs” (asymmetry, border irregularity, multiple colors, larger diameter, and evolution or change) of melanoma AND
- Modified ABCDEs of pediatric melanoma—Amelanotic (lack of color/pink); Bleeding or raised; Color uniformity; Arising De Novo (new spot); Evolving (changing)
- Pediatric melanoma can look like a lot of other common and benign (not cancerous) skin condition like warts and pyogenic granulomas (vascular bumps)
- Other pointers—look for pink or yellow bumps that itch or bleed AND look for the ‘ugly duckling’ spot
How can you help your child or teen?
Practice sun safety measures to limit UV radiation damage:
- Avoid the sun/outdoors between 10-4pm
- Seek shade when outside and stay covered
- Never allow your child to use indoor tanning devices
- Keep children under 6 months of age covered and out of the sun
- Use a broad spectrum, water resistant sunscreen, with spf 30 or higher and reapply every 90 minutes, and more when sweating or swimming
- Use sun protective clothing, including sunglasses, a broad brimmed hat, and UV protective clothing with ‘UPF’ labels, and don’t forget those swim shirts!
What to do if you are worried your child may have melanoma?
Get to a board-certified dermatologist or pediatric dermatologist right away. Pediatric dermatologists are further specialized to know how melanomas may present in young children and are familiar with the best techniques to safely biopsy a skin lesion on your child, if this is indicated. At Phoenix Children’s Hospital we have a specialized care team of several physicians from the divisions of dermatology, oncology, genetics, plastic surgery, pathology and pediatric surgery, to help care for patients with melanoma. These doctors work as a team and review your child’s medical information and test results and will discuss a plan for management and treatment with your family. At Phoenix Children’s Hospital, this team utilizes the latest medical information, clinical trial data and technology, to ensure we offer your child the latest advancements in melanoma treatment and care.
How is melanoma treated in children?
Melanoma is usually removed by a surgeon subspecialized in pediatrics. If it has spread to other parts of the body, your child may be treated with additional surgery and immunotherapy. Immunotherapy works by unleashing the body’s immune system to attack the cancer cells. About 50% of melanomas have genetic mutations called BRAF mutations that makes it possible to treat the melanoma with personalized targeted medicines.
The Phoenix Children’s Center for Cancer and Blood Disorders is at the forefront of cancer research. We have more clinical trials than any other pediatric hospital in the state of Arizona and a dedicated group of pediatric oncologists who are experts in melanoma.

