Multimodality neurologic monitoring in the neurocritical care unit is a method of continuous monitoring for brain and body function using different tools in a single patient. This form of monitoring for brain injury is being increasingly recognized as useful tool in clinical decision support in the neurocritical care field. It represents an extension of the neurologic examination and clinical skill set of bedside clinicians to better understand brain physiology in real time for unstable critically ill patients who may be comatose.

The fundamental goal of multimodality neurologic monitoring is to detect early signs of brain injury or worsening brain injury before irreversible brain damage takes place.
To that end, it adds value in:
- Detecting early signs of brain injury before irreversible brain damage takes place
- Allowing the clinical team to set individualized goals for blood pressure, intracranial pressure and ventilation management for optimal brain health
- Monitoring the response of therapies administered
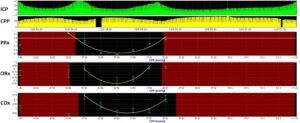
- Enhancing clinicians’ understanding of cerebral autoregulation, brain compliance, and autonomic function in real time
- Aiding in the design and implementation of management protocols
By adding value in this manner, the fundamental goal of this strategy is to help in improving outcomes and quality of life for survivors of critical brain injury.
The Challenge
Secondary brain injury can result in the hours and days after initial injury because of changes in cellular injury cascade or secondary brain insults such as increased intracranial pressure, poor ventilation or lack of sufficient blood flow to the brain. Despite standard guidelines for blood pressure, intracranial pressure or ventilation parameters established for patients with acute injuries, every patient is unique and may require their own distinct hour-to-hour parameters for goals of care. There is need to better understand the goals that every individual child needs to optimize brain health during critical illness.
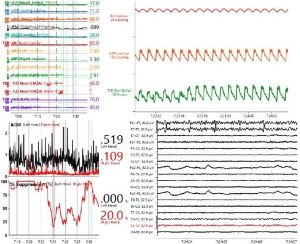
Multiple modalities can be used to monitor for secondary brain injury, including continuous electroencephalography, transcranial Doppler ultrasound (CD), pupillometry, brain tissue oxygenation monitoring, and intracranial pressure (ICP) monitoring. Each modality, in isolation, gives a limited window into real-time brain physiology. By combining these tools in real-time, clinicians are able to have broader insights into brain pathophysiology. Furthermore, advanced calculation of model-based indices of cerebral autoregulation, brain compliance and autonomic function allow physicians to better understand what specific parameters may be used in care to promote optimal brain health and recovery.
Currently, there are only a handful of pediatric and adult centers that integrate multimodality neurologic monitoring into routine patient care because of the requirement of advanced technology and expertise to use and implement these tools in real-time.
Real-Time Analysis at Barrow Neurological Institute at Phoenix Children’s
The Neurocritical Care Program at Barrow Neurological Institute at Phoenix Children’s utilizes a total of six multimodal monitoring units that are available for use within the hospital’s pediatric, cardiac and neonatal intensive care units. These devices time synchronize all brain and systemic monitoring tools at high resolution with raw waveforms available for analysis. The data is archived into a clinical database capable of storing this data, and network ports are available for streaming the data in real-time over the hospital network so that clinicians both at the bedside, as well as in the operating room or throughout the hospital can look live at changes in brain physiology for their patients. Using advanced software, the data can be used to calculate model-based indices of cerebral dynamics that allow physicians to understand, at any given time, what may be a patient’s clinical state as well as their optimal cerebral perfusion pressure, blood pressure, ventilator settings, or critical closing pressure. Furthermore, a structured process has been developed to provide clinical teams with standardized reporting of these measurements, as well as ascertaining the dose and percent time that goals of care were achieved, as well as the degree in which specific therapies are effective in improving care.
Research and Future Directions
The ability to collect and store high-resolution physiologic data of children either with acute brain injury or at risk of such injury allows a unique opportunity for scientists to investigate for biomarkers of worsening brain injury, brain recovery, and treatment efficacy that are not yet well established, but may hold promise in helping children in the future. At Barrow Neurological Institute at Phoenix Children’s, we have successfully acquiring funding of investigator-initiated proposals from both federal and local agencies understand biomarkers of brain injury and clinical recovery from this data.
These include:
- A U.S Department of Defense Epilepsy Research Program Award to study biomarkers of post-traumatic seizures and post-traumatic epilepsy in children with severe traumatic brain injury
- An American Heart Association Career Development Award to study biomarkers of acquired injury in children undergoing mechanical circulatory support
- Two awards from the University of Arizona Valley Research Partnership program and the Innovators in Neuroscience in Kids Foundation to study physiologic biomarkers of covert consciousness in the ICU after acute brain injury
We actively publish peer-reviewed articles to better understand these biomarkers of brain insults and brain recovery in children. Recent publications include:
- Appavu B, Foldes S, Burrows BT, Jacobson A, Abruzzo T, Boerwinkle V, Willyerd A, Mangum T, Marku I, Adelson PD. Multimodal Assessment of Cerebral Autoregulation and Autonomic Function after Pediatric Cerebral Arteriovenous Malformation Rupture. Neurocritical Care. [In Press, 2020]
- Appavu B, Foldes S, Temkit M, Jacobson A, Burrows BT, Brown D, Boerwinkle V, Marku I, Adelson PD. Intracranial Electroencephalography in Pediatric Severe Traumatic Brain Injury. Pedatr Crit Care Med. 2020 Mar;21(3):240-247. PMID: 31569184.
- Appavu B, Burrows BT, Foldes S, Adelson PD. Approaches to Multimodality Monitoring in Pediatric Traumatic Brain Injury. Front Neurol. 2019 Nov 26;10.1261. PMID 32038449.
- Appavu B, Foldes ST, Adelson PD. Clinical trials in pediatric traumatic brain injury: definition of insanity? J Neurosurg Pediatr. 2019 June 1:23(6):661-669.
As more and more pediatric and adult neurocritical care centers adopt multimodality neurologic monitoring in both clinical care and through research, we look to harness and strengthen our collaborations both nationally and internationally to conduct larger prospective studies to investigate for biomarkers of worsening brain injury and clinical recovery. Overall, the future is bright for finding novel ways of improving care for critically ill-children.
