Colorectal Clinic for Children: Bowel Management, Surgery & Care
At the Phoenix Children’s Colorectal Clinic, our specialists use the latest surgical and minimally invasive techniques to help children with a wide range of colorectal and pelvic conditions. Everything we do is carefully planned around your child’s unique needs to restore healthy bowel function and help them feel more comfortable and confident.
Family-Centered Care
We know your child’s colorectal issues affect every aspect of your family’s life. We offer a wide range of programs and services designed to help you navigate your child’s physical, emotional and behavioral health challenges.
Our team of experts provides guidance and helps you understand each step of your child’s care. If your baby has a diagnosis of an anorectal malformation, cloaca or exstrophy, you may find it helpful to talk to other families with similar experiences. They can answer your questions and help reduce any anxiety or stress you may feel. Once your child is diagnosed, we can introduce you to families that have had similar experiences who can offer insight and support.
Our clinic offers workshops for patients and their families interested in education, personal connections and giving and receiving support. These peer support parties and workshops feature brief informational sessions and age-appropriate breakout groups. Clinic physicians and staff are available to offer support, encouragement and answers to your individual questions. We also plan parties and events so patients and families can get to know each other, relax and have fun outside the hospital.
Children with colorectal conditions often face unique challenges in school. We educate teachers about the needs of children with bowel or bladder reconstructions. We are happy to advocate for accommodations for your child with school administrators, nurses or educators. We can also connect you with other parents and advocacy groups who can help guide you.
Every child is different in terms of how and when they poop. We discuss using positive potty-training techniques when the time is right. We work with each child to advocate for themselves at school to ensure they receive their scheduled bathroom breaks.
Common daily challenges and unexpected events can affect your ability to care for your child with a medical condition. In addition to surgical procedures, we connect you with the services, support and resources you need. The right services and support help your child achieve good outcomes and a high quality of life.
Bowel Management
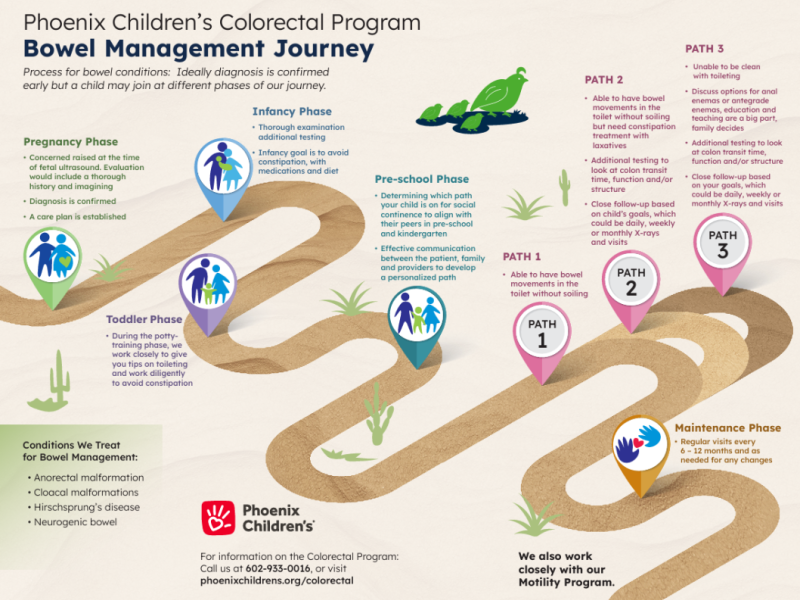
When you come to us for help with your child’s bowel management, we’ll start with a thorough history of your child’s bowel function.
Your child may need additional testing, which could include:
- Abdominal X-rays: stool burden, obstructions and the cause of your child's pain
- Anorectal manometry: Evaluate your child’s anal and pelvic muscle strength and sensation
- Colonic manometry: Measure how strongly your child’s large intestine contracts
- Contrast enema imaging: Shows the structure of your child's large intestine and rectum, using an X-ray that uses water-soluble contrast
- MRI of the spine: Look for associated conditions and vertebral abnormalities
- Exam under anesthesia (EUA): Assess prior surgical repairs or obtain rectal biopsies while your child is asleep under anesthesia
Treatment options may include:
- Dietary fiber and hydration
- Oral medications, including laxatives, fiber supplements or medications to treat diarrhea
- Large-volume rectal enemas, including Navina, Peristeen® and the Foley catheter system
- Antegrade enemas, including Malone antegrade continence enema (MACE), Neo-Malone, Chait cecostomy tube and MiniACE® cecostomy tube
- Redo surgery when indicated
At the beginning of your child's bowel management journey, we will closely follow your child's symptoms. We schedule appointments daily, weekly or monthly, depending on the type of intervention, your goals and your schedule. We connect every six to 12 months to answer any questions and address any new or ongoing concerns.
Procedures
At the Phoenix Children’s Colorectal Clinic, our team of pediatric specialists uses the latest surgical and minimally invasive techniques to address a wide range of colorectal and pelvic conditions. Every procedure is carefully planned around your child's unique needs to restore healthy bowel function and help them feel comfortable and confident.
An antegrade continence enema is also called an ACE enema. It is used to help someone with constipation or incontinence. A standard enema puts liquid into the rectum to help release stool from the last portion of the large intestine. In many cases, this type of enema is an effective treatment for constipation.
In an ACE, an opening is created surgically from the abdomen into the large intestine. This allows the enema fluid to enter the body at the beginning of the large intestine and push the stool out of the body in a more natural way. They are most often used in children who need long-term bowel management therapy.
There are two types of ACE:
- Appendicostomy (Malone procedure): Allows the patient to empty their bowels using an enema administered through a small tube typically in the belly that leads into the large intestine.
- Cecostomy: Surgeons create a surgical opening so a tube can be placed to flush the large intestine. Once the tube is in place, liquid medicine can be injected into the first part of the large intestine (cecum).
Antegrade Enema Options - English Watch the video
Antegrade Enema Options - Spanish Watch the video
Using a Cecostomy Bag Watch the video
Laparoscopic anorectoplasty is a minimally invasive surgery used to correct certain types of high anorectal malformations, where a child’s rectum and anus don’t develop normally.
During the procedure, surgeons use small incisions and a tiny camera to create or reposition the rectum and connect it to the anus, allowing the stool to pass normally.
Posterior sagittal anorectoplasty (PSARP) is a procedure used to correct anorectal malformations, where a baby’s rectum and anus haven’t formed or connected properly. During the procedure, the surgeon creates a new anal opening, allowing your child to pass stool via their neo-anus
Our surgical management of cloaca includes:
- Rectal exam under anesthesia (EUA): A doctor examines your child’s rectum and surrounding area while the child is asleep under anesthesia, allowing for a thorough and pain-free assessment to check for abnormalities or plan surgical treatment.
- Posterior sagittal anorectal vaginal urethral plasty (PSARVUP): Reconstructive surgery used to correct cloaca, a condition where the rectum, vagina and urinary tract share a single opening. During the procedure, surgeons separate and rebuild these three structures so that each has its own standard opening. The rectum is then connected to a newly created anus.
Pull-through surgery for Hirschsprung disease is a surgical procedure to remove the section of the large intestine that is unable to move stool normally due to a lack of nerves. Surgeons then “pull through” the healthy part of the intestine and connect it to the anus, allowing the child to pass stool. This surgery helps relieve severe constipation and restore normal bowel function.
A rectal examination under anesthesia (EUA) with cystoscopy, vaginoscopy and cloacagram is a set of tests done while your child is under anesthesia to carefully evaluate their pelvic organs and structures.
During the procedure, doctors will examine the structures and assess their relationship to each other. These tests help us fully understand your child’s anatomy before planning complex reconstructive surgery.
This test can either be done in the clinic as a procedure if your child is a baby or while your child is under anesthesia if they are older to check whether nerve cells are present in your child’s rectal tissue. The test is often used to diagnose conditions such as Hirschsprung disease, where part of the intestine lacks nerves.
Rectal prolapse repair surgery is a procedure to fix the rectum when it slips out of the anus (rectal prolapse). This can include both rectal sclerotherapy and surgical fixation.
During the surgery, doctors move the rectum back into its normal position. They may secure it in place with stitches or remove a small portion if needed. This helps relieve symptoms such as pain, bleeding and stool leakage, and prevents the prolapse from recurring.